Sexually Transmitted Infection
Protecting yourself from sexually transmitted infections (STIs) involves a combination of knowledge, safe practices, and regular testing. Here are some essential steps:

Safe Sex Practices
- Condoms: Always use a latex condom during vaginal, anal, or oral sex. Condoms act as a barrier and significantly reduce the risk of STI transmission.
- Dental Dams: For oral sex, use a dental dam to protect against STIs.
- Limit Sexual Partners: Reducing the number of sexual partners lowers your exposure to potential infections.

Make a Donation
Every contribution, no matter the size, makes a significant impact. Your donation will help us continue providing high-quality services to those who need them most.
Become a Sponsor, Advocate, Partner and or leave a Gift for MyHealthnet in your Will.
DonateRemember, knowledge and proactive steps are your best defence against STIs. Regular testing and safe practices are essential for maintaining sexual health.
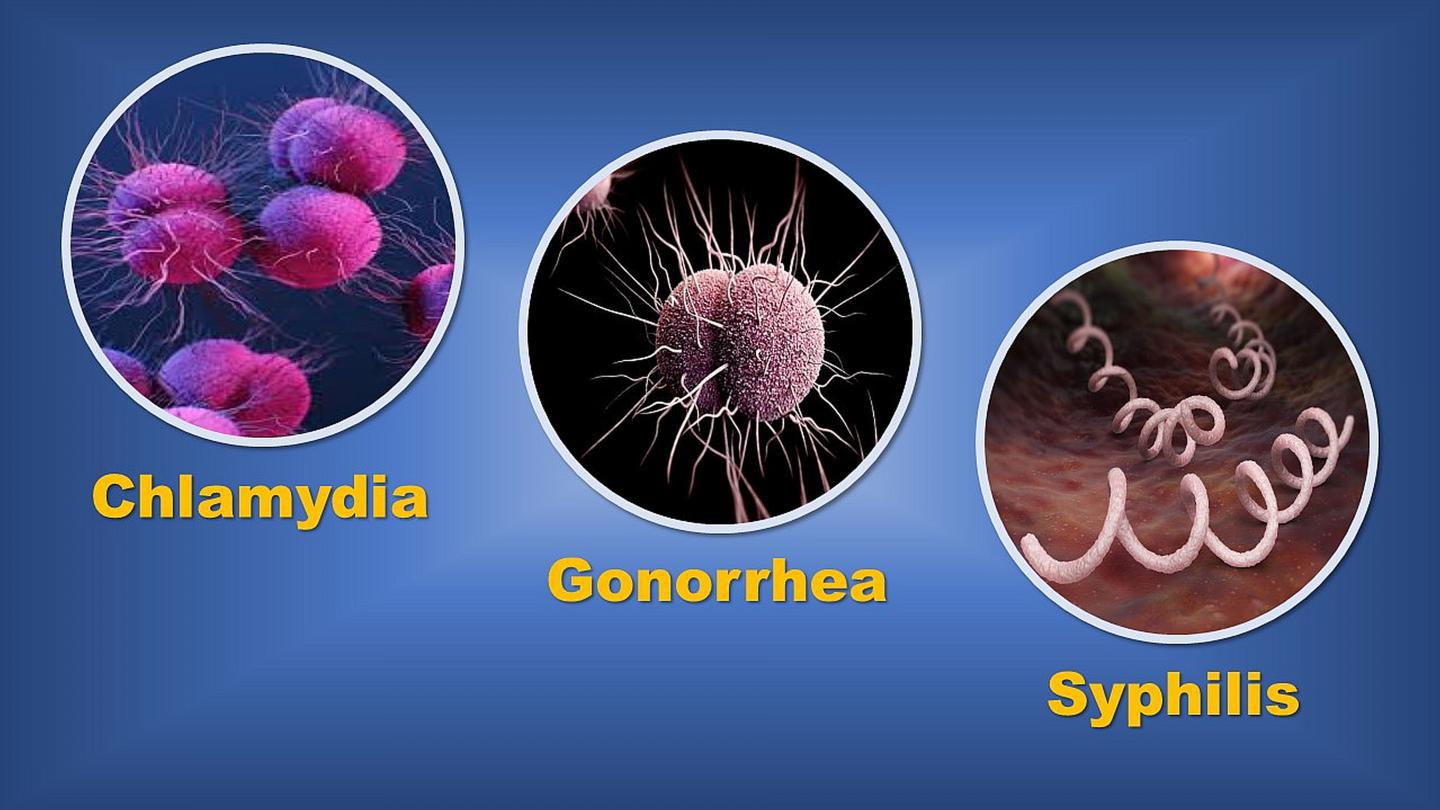
Common sexually transmitted infections (STIs):

Genital Herpes
- Symptoms can appear after 4 to 7 days but might not start until months or years later.
- Common symptoms include:
- Small, painful blisters around the genitals
- Pain when urinating
- Tingling or itching around the genitals

Genital Warts:
- Symptoms could start from 3 weeks to many months or even years after contact with the virus.
- Common symptoms include:
- Small, fleshy growths or bumps on the genitals or around the anus (usually painless but may be itchy)
- Most people with the virus that causes genital warts do not develop obvious warts.

Gonorrhoea
- Symptoms usually appear within 2 weeks of being infected but could start much later.
- Common symptoms include:
- Green or yellow discharge from the vagina or penis
- Pain when peeing
- Lower tummy pain
- About 10% of men and 50% of women who are infected do not have any symptoms.

Syphilis
- Symptoms usually appear after 2 to 3 weeks but could start earlier or much later.
- Common symptoms include:
- One or more small, painless sores or ulcers on the genitals
- A blotchy rash, white patches in the mouth, and flu-like symptoms that may follow a few weeks later
- Symptoms are often not obvious and may come and go.

Trichomoniasis:
- Symptoms usually appear within 4 weeks but could start months later.
- Common symptoms include:
- Unusual discharge from the vagina or penis
- Pain or burning when peeing
- Itching and redness in the genital area
- Trichomoniasis is more common in women

Pubic Lice (Crabs STD)
Pubic lice, commonly known as "crabs," are parasites that inhabit the pubic hair and are typically spread through close personal contact.
- Pubic Lice (Crabs) Symptoms
- Severe itching
- Visible crawling lice or eggs attached to pubic hair

Scabies
Scabies is a disease caused by lice infestation.
- Scabies Symptoms
- Extreme itching that is worse at night.
- The skin appears to have a pimple-like rash, as shown in this photo.
- Both the itching and rash may be across the body or limited to the wrist, elbow, armpit, webbing between fingers, nipple, penis, waist, belt-line or buttocks.
- Tiny blisters (vesicles) and scales may appear.
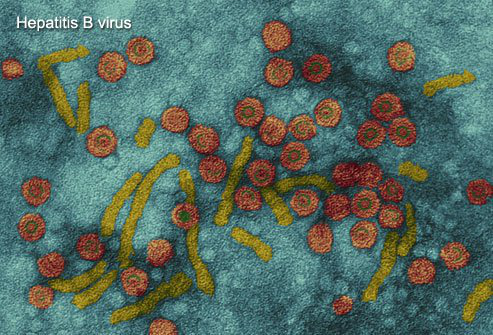
Hepatitis B
Hepatitis B is a virus that spreads through contact with body fluids and blood, so it can be transmitted through sexual intercourse.
- Hepatitis B Symptoms
- Nausea
- Abdominal pain
- Jaundice (yellowing of the skin and whites of the eyes)
- Over time, scarring of the liver (cirrhosis) and liver cancer can develop
- Although there is no cure, there is a vaccine to prevent hepatitis B infection.

HIV/AIDS Virus
The HIV Virus (AIDS virus) weakens the body's immune system. It is spread through sexual contact, needle sharing, or from an infected mother to a baby.
- HIV Symptoms
- Flu-like symptoms 1 to 2 months after the first infection, including swollen lymph nodes, fever, and headaches
- Chills
- Rash
- Night sweats
- Muscle Aches
- Sore throat
- Swollen lymph nodes
- Mouth ulcers
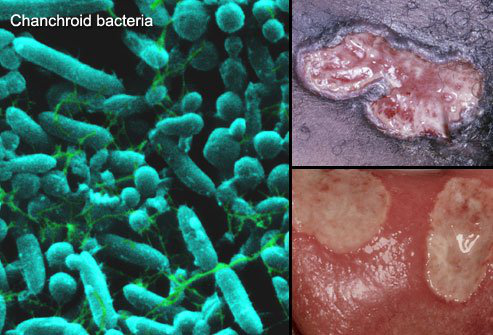
Chancroid (STD)
Chancroid is an STD that is rarely seen in the UK. It is more common in Africa and Asia. It causes painful lumps in the genital area that can progress to open sores.
- Chancroid Symptoms
- One or more sores or raised bumps on the genitals. A narrow, red border surrounds the sores. The sores become filled with pus and eventually rupture into a painful open sore.
- About half the time when untreated, the chancroid bacterial infection spreads to the groin’s lymph glands, causing the groin to enlarge and become hard and painful.

Lymphogranuloma venereum (LGV)
Lymphogranuloma venereum (LGV) is a type of chlamydial infection, but it is caused by a different type of chlamydia (Chlamydia trachomatis) than the usual chlamydial STD.
- Early Symptoms
- Soft red, painless sores on or near the genitals or anus
- Similar sores in the throat or mouth following oral sex
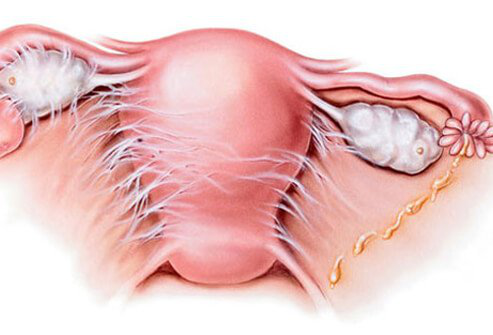
Pelvic Inflammatory Disease
Pelvic inflammatory disease (PID) is not a specific STD. Rather, it is a complication that can develop following multiple different STDs, particularly gonorrhoea and chlamydia.
- PID Symptoms
- Fever
- Pelvic or low abdominal pain
- Painful urination
- Discharge
- Painful intercourse
Untreated sexually transmitted infections (STIs) can have serious long-term consequences. Let’s explore some of these effects:
Genital Herpes
Long-term complications include:
- Male and female sterility
- Blindness
- Bone deformities
- Damage to major organs (heart, kidney, brain, etc.).
Chlamydia
If left untreated, Chlamydia can lead to:
- Pelvic inflammatory disease (PID) in women, causing damage to the reproductive organs and increasing the risk of infertility.
- Ectopic pregnancy, where the fertilised egg implants outside the uterus.
- Inflammation of the testicles (epididymitis) in men, which can cause pain and swelling.
- Reactive arthritis, affecting both men and women.
While waiting for your partner’s decision regarding STI testing, it’s essential to prioritize your health and well-being. Here are some steps you can take to protect yourself:
Abstain from Sex
- Since STIs can spread through skin-to-skin contact or bodily fluids, consider abstaining from sexual activity while awaiting results.
- If you do decide to have sex, use a physical barrier such as a condom or dental dam to protect your partner1.
Educate Yourself
- Learn about suitable contraceptive methods, signs and symptoms of STIs, and the benefits of regular STI angle-double-right-ups.
- Being informed empowers you to make safer choices when sexually active.
Remember that your health matters, and taking proactive steps can help prevent the spread of STIs. If you have any concerns, seek advice from a sexual health clinic or healthcare provider. Stay informed and take care!
Partner Notification (PN)
PN is a crucial aspect of managing sexually transmitted infections (STIs) in the UK.
What Is Partner Notification?
- Partner notification involves reaching out to previous sexual partners who may be at risk of the same STI. The goal is to encourage them to get tested and, if necessary, receive treatment.
- By notifying partners, we can:
- Prevent reinfection.
- Reduce the transmission of STIs.
- Ensure timely testing and treatment for partners.
How Does PN Work?
If you’ve been diagnosed with an STI, consider the following steps:
- Health Advisors: Seek assistance from health advisors at sexual health clinics. They can help you inform your partners without revealing your identity.
- Anonymous Text Messages: Many UK sexual health clinics offer a free electronic partner notification service. This service sends anonymous text messages to your sexual partners, notifying them of potential exposure to an STI. No more awkward individual contacts—technology does the work for you!
Why Is It Important?
- Preventing Spread: Partner notification prevents the spread of STIs by ensuring that partners get tested promptly.
- Health Complications: Early testing and treatment prevent health complications for both you and your partners.
If you suspect an STI, seek advice from MyHealthnet, and get a sexual health test at a clinic. They can provide accurate diagnosis, treatment, and guidance on partner notification. Stay informed and take care! Book an appointment to speak to experts. Join our experts.
Help Someone with an STI Diagnosis
Supporting someone who has received an STI diagnosis is crucial. Here are some ways you can be there for them during this challenging time:
Listen Actively and Non-Judgmentally
- Be an empathetic listener. Let them express their feelings without interruption.
- Avoid using labels or making assumptions. Be sympathetic and non-critical.
Educate Yourself
- Learn about STIs. Understand the specific infection they’re dealing with.
- Research symptoms, treatments, and prognosis. This knowledge will help you empathize and provide informed support.
Understand the Emotional Impact
- An STI diagnosis can evoke a range of emotions: fear, shame, anxiety, and loneliness.
- Acknowledge their feelings. Let them know it’s okay to feel overwhelmed.
Respect Their Privacy
- Keep their diagnosis confidential. They may only want to discuss it with trusted individuals.
- Assure them that what they share with you won’t go further.
Avoid Offering Solutions
- Sometimes, just listening is the most powerful support you can provide.
- Avoid pushing solutions or advice unless they specifically ask for it.
Be There for Them
- angle-double-right in regularly. Loneliness can exacerbate the emotional impact of an STI.
- Offer your presence, whether through calls, texts, or in-person visits.
Remember, your kindness and understanding can make a significant difference during this challenging time.
My Partner Refuses to Get Tested
If your partner refuses to get tested for sexually transmitted infections (STIs/STDs), it can be challenging, but there are steps you can take to address the situation:
When to Bring Up Conversations About STIs/STDs Testing
- Ideally, discuss testing before engaging in sexual activity. Open communication is essential.
Inquire About the Real Reasons
- Ask your partner why they are hesitant. Understanding their concerns can guide your approach.
Keep a Clear Head and Avoid Judgment
- Stay calm and non-judgmental. Remember that everyone has their reasons.
Discuss Logically by Sharing Facts
- Share information about the importance of testing, potential risks, and the benefits of early detection and treatment./li>
Simplify the Hassle
- Offer to accompany your partner to a sexual health clinic or testing centre. Make it easier for them.
Explain Your Testing History
- Share your own experiences with testing. Talk normally about the process.
Empower and Reassure Your Partner
- Use comforting words. Let them know that getting tested is a responsible and caring choice for both of you.
Remember that you do not have to engage in intercourse to pick up an STI, oral sex and kissing can also transmit infections. If your partner remains unwilling, prioritise your health, and consider abstaining from sexual contact. Ask for advice from our experts, or visit your local sexual health clinic for further guidance and support.
Who's at Risk for STDs?

It's estimated that half of sexually active young adults acquire an STD by age 25. In fact, STDs are the most common type of infection in America. While STDs are more common in teens and young adults, anyone who is sexually active is at risk. The risk is raised by having multiple sex partners. The incidence of some STDs, including LGV and syphilis, is rising in men who have sex with men.
Can Virgins Get STDs?

Many STDs can spread through any type of sexual activity. This includes skin-to-skin contact and oral sex. This means that people who have not yet had sexual intercourse can still get STDs.
STD Prevention

Abstinence from any sexual contact is the only absolute way to prevent getting an STD. Being in a long-term, monogamous relationship also is a good way to avoid STDs. There are also steps you can take to decrease the chance of getting an STD if you are sexually active, including:
- Asking partners if they have ever had an STD
- Using condoms
- Avoiding sexual activity with a partner who has signs of an STD
- Asking partners to be tested before having sex
- Being aware of symptoms and signs of STDs
How to Tell Your Partner You Have an STD

It may be difficult, but it is important to tell your partner as soon as possible if you believe you may have an STD. Even if you are being treated, you may still be able to spread the infection. For some STDs, it's recommended that both partners be treated at the same time.
It can be difficult to share this information, so some people find that preparing a script in advance can be helpful. Here are some facts that can help the conversation go more smoothly:
Discovering an STD is not evidence of cheating. It may very well have come from one of yours or your partner’s past relationships.
An estimated one in two sexually active people will contract an STD by the time they reach age 25. Most of these don’t know they have an STD. Many STDs show few or no symptoms when contracted and may be discovered much later.
It’s normal to be nervous about this topic. But by being bold and taking action, you can actively promote better health for you and your partner.
STDs and Pregnancy

STDs can cause premature labour in pregnant women, and many STDs can be passed to the baby either during pregnancy or childbirth. So, all pregnant women should be checked for STDs.
STDs can cause numerous problems in babies, like low birth weight, stillbirth, nerve problems, blindness, serious infections, and liver problems.
Treatment during pregnancy can reduce the risks of these complications and can cure many types of infections.
Can STDs Come Back?

In most cases, new exposures to STDs that you have had in the past can cause you to get the infection again. Most treatments don't protect you from developing the STD at a future time. If your partner has not been treated, you may pass the infection back and forth. Without the right precautions, you could acquire a second STD or a recurrence of the same infection. In addition, genital herpes virus infections can be recurrent after a single exposure.
Some experts prefer to term STDs as STIs (sexually transmitted infections). STIs include all infections that can be transmitted sexually. For example, scabies and most recently, Zika virus infections are better classified as STIs.
Have a query and or need more information?
STD Diagnosis, Tests Images, Symptoms, Treatment and or wish to support MHN or tell your story.
Book an appointment to speak to an advisor if you think you have an STD/STI, or about related enquiries.




















Comments